If you’ve opened a magazine, scrolled through TikTok and Instagram, or turned on the news over the past year, you’ve probably heard about the latest weight-loss craze: Ozempic, an injectable medication that everyone from red-carpet celebrities to your neighbors seem to be taking to shed pounds.
Ozempic is a name brand for the drug semaglutide, initially used just for patients with diabetes. But the medication had a side effect—weight loss—and it’s not just people in Hollywood who took notice. Liza Moore, a dermatologist and internist near Tysons who started offering medical weight-loss shots at her practice in March, says she now sees multiple clients a day for the treatments.
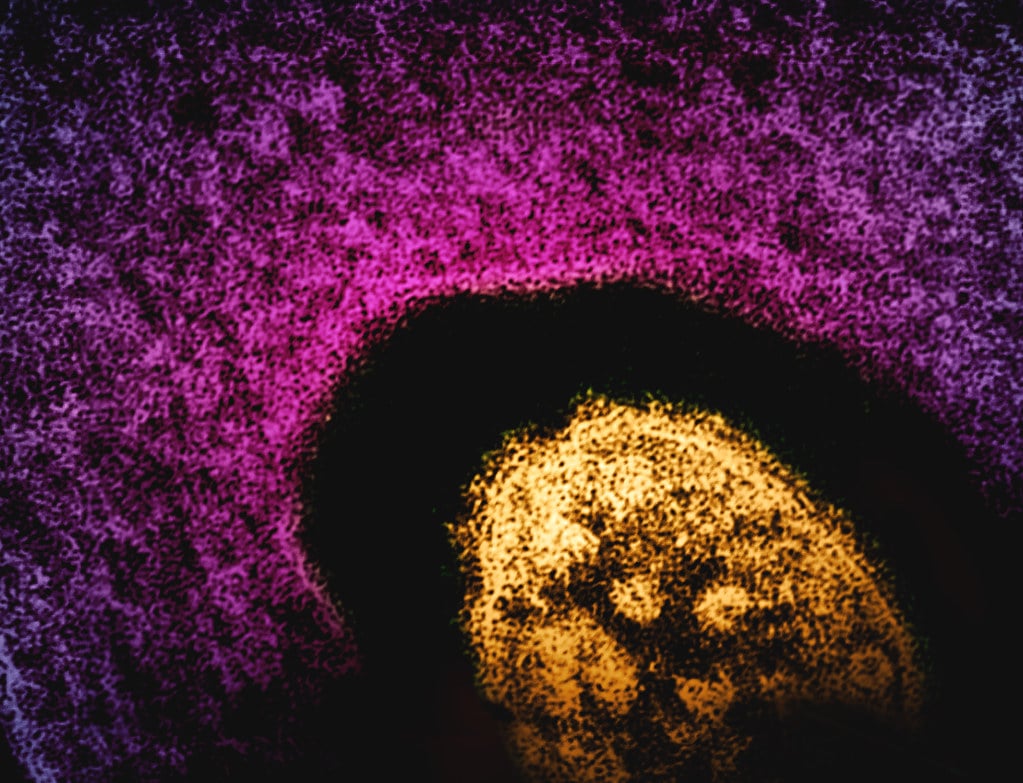
“Why these medications work so well and they’re so popular is that they suppress appetite centers in the brain,” says Gerti Tashko, an endocrinologist in Rockville. “So there is less hunger and appetite, which makes [patients’] journey of weight loss easier to follow.”
How does the drug work? Semaglutide stimulates insulin production and lowers blood-sugar levels, mimicking glucagon-like peptide-1, a hormone that signals fullness and slows gastric emptying. As a result, people eat less.
“You’re Going to Feel Like You Ate a Thanksgiving Meal”
Ozempic, the most commonly known semaglutide shot, is a weekly injection approved by the FDA for diabetes treatment and used off-label for weight loss. Meanwhile, Wegovy, another weekly injection with a larger maximum dose, was FDA-approved in 2021 for weight management in patients with a body-mass index of 30 or more, or a BMI over 27 with weight-related health issues.
Among the medications’ side effects are nausea after the initial injection and, for some, GI-related problems such as constipation or diarrhea.
Often, those taking the medication are well versed in weight-loss strategies. “I would say 95 percent of our patients are people who have tried and failed other methods,” says Moore. “They’ve done Jenny Craig, Weight Watchers; they’ve done the gym thing with a personal trainer.”
Prior to offering the shot, Moore saw patients coming into the office for Morpheus8—a radiofrequency treatment that tightens skin on the face and body with the use of microneedles—after weight loss with Ozempic. Moore decided to add medical weight loss to her treatment roster, to pair with procedures such as CoolSculpting and filler after the pounds are shed. “We’re like, ‘Just wait—once you start the Ozempic, you’re going to feel all day like you just ate a Thanksgiving meal,’ ” says Moore.
Not So High on Sugar
Lily Talakoub, a dermatologist at McLean & Potomac Dermatology, has many patients—mostly women 30 to 55—who have hit a plateau in their weight loss. She initially administered semaglutide medications to treat skin diseases triggered by insulin resistance. In addition to seeing the skin conditions clear, patients reported weight loss and improved mood. Talakoub started offering the treatment about eight months ago specifically for weight loss, and word spread, bringing in lots of new patients. “I can’t even count how many,” she says.
Talakoub notes that beyond suppressing appetite, the medication is helping patients change their underlying behavior: “One of the things that I found the semaglutide does is it teaches people what they can and cannot eat. On the medicine, if you eat something that’s too sugary, if you eat something that’s too heavy, you’re not going to feel right. That’s a really good feedback loop for patients.” Moore’s patients also report fewer cravings as well as discomfort after eating certain foods, which helps them overhaul their diets. “They’re focusing more on ‘what’s good to put inside my body’ instead of ‘what is my body craving,’ ” she says.
But food isn’t solely fuel—it’s also a source of pleasure. People taking semaglutide may experience an aversion to once-favorite foods or find themselves able to stomach only a few bites of a meal, disconnected from a previous sense of joy. Says DC plastic surgeon Troy Pittman: “The pleasure centers we get when you see a little kid walking down the sidewalk eating a big ice-cream cone, and you’re like, ‘Oh, that looks good, I’m going to have that because it’ll make me happy’—all of that gets blunted.”
Sober-Curious
Behavioral changes aren’t limited to eating. Doctors report that patients are cutting back on drinking while taking the medication. It’s not that they can’t drink—it is just not as tempting.
“Because you’re blunting a pleasure center, you don’t have cravings for all of the other things that bring you pleasure,” says Pittman. “A lot of patients are losing weight because they’re not drinking alcohol.” That includes wine, with its high-sugar content, and carb-heavy beer, which is less appealing when you hit satiety quicker. “They’re like, ‘I don’t even feel like drinking, and even if I have a glass of wine, I don’t feel good when I have it.’ ”
Once patients reach their goal weight, says Tashko, the endocrinologist, he lowers the dose—but relies on patients to speak up when challenges lie ahead. “They tell me, ‘I have high stress levels at my job currently, I have these parties coming or celebrations—I need some assistance because I know I will relapse,’ ” says Tashko. “And then we might we go up a little bit on the dose temporarily.”
It isn’t known whether the suppressive effects can be applied to behaviors beyond eating, and clinical trials are in progress to see whether the drugs can also curb smoking.
Hunger Pains
Although weight loss can help lower blood pressure and cholesterol, there are health risks to consider while on the medication. Pittman, who doesn’t prescribe medical weight-loss drugs but works with people taking them, shares the story of a patient who constantly felt nauseated while taking the medication. Her not-so-healthy way of combating nausea? Consuming a single piece of candy—a sign to Pittman that she was likely struggling with low blood sugar. He’s concerned about the long-term consequences of drastically cutting back on food—from losing muscle mass to slowed wound healing—that he believes get lost in the hype.
Pittman points to “Ozempic face”—the term for what happens when cheek skin begins to sag while a patient is taking semaglutide—as an example of how people are disconnected from the drug’s effect on the body: The phenomenon isn’t a side effect of the medication itself but a consequence of not eating. “Anytime someone has rapid weight loss, they’re going to have facial wasting,” he says. “You could rebrand it as ‘gastric-bypass face,’ you could rebrand it ‘terminalillness face.’ ”
In an effort to mitigate such consequences, the doctors we spoke to who are administering the medication say they track patients closely. Talakoub sees her medical-weight-loss patients each week to monitor symptoms and dosing, and Christie Youssef, a lifestyle-medicine physician at Kaiser Permanente, stresses the importance of using the medication as part of a larger health plan. When her patients are prescribed Wegovy or Saxenda, another weight-loss drug, they work alongside a nutritionist and coach to develop healthy habits for sustained weight loss. She’s hoping for more longitudinal studies that look at how weight loss is maintained over time using these medications. Meanwhile, her patients are armed with advice on nutrition, fitness, sleep, and more to supplement the medical weight loss.
“Yes, these medications are a tool,” says Youssef. “But they have to be coupled with all the other things we have in our toolbox.”
This article appears in the July 2023 issue of Washingtonian.