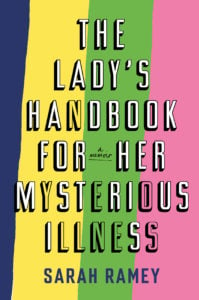
Dear Reader,
There may exist a graceful and elegant way to begin one’s gynecologic and colorectal memoir, but it never does spring to mind.
Let us start then with a story. We can travel back to where it all began, and for a moment leave the particulars behind. That sounds much nicer—lovely even—considering it all began so many years ago with a cool, luxuriant swim in Walden Pond.
I remember it well. The heat was heavy, I was a summer student at Harvard with no air conditioning, and Walden beckoned for the reasons it always will. Though I suppose the busloads of tourists beached on the imported sand should have sounded some instinctive alarm when I arrived, they didn’t. I walked right on past and made my way to the side of the pond where the water was still and the snorkelers out of sight.
I remember walking into the water. I remember floating on my back. I remember the coolness and the peace and the poetry of the place, and I remember feeling like I couldn’t ask for anything more.
The next day in the emergency room, I had quite forgotten all of that.
A urinary-tract infection, known as a UTI, is a very painful but easily treatable infection of the urethra. Most people describe it as “peeing broken glass,” and I would have to agree with most people.
But my ER doctors patted me on the back as they ordered the standard antibiotics and I bounded off to the pharmacy, clutching my prescription, counting the minutes in the 24 hours they told me it would take to go away.
Fifty-six hours later, I was back in the emergency room. It had not gone away.
In fact, it did not go away for six months. “How strange,” the college physician said as he took my history. I had never been sexually active, which made things particularly challenging, both diagnostically and emotionally. I was a senior in college, and it was my time. I even had the right person picked out.
But the UTI stayed. We joked and called it my PUTI, or permanent UTI, and I laughed along with the rest. But in private, in the bathroom, I was profoundly unamused.
This prologue is typical of women like me. A simple and innocuous medical event—often with a gyno or gastro tilt—that should have resolved simply but didn’t. She thinks it is just another one of life’s ups and downs, when in fact Up is about to become a distant memory.
There is a secret society of sorts that no one—not even any member—has heard of. We don’t look alike, we don’t dress alike, and we’re from all over. There is no secret handshake, no meeting place, no cipher.
We are the women with mysterious illnesses, and we are everywhere.
When I went home for Christmas in Bethesda, my parents—who are both top-notch physicians—made an appointment for me to see Washington’s preeminent, top-notch urologist.
Dr. Damaskus said I seemed like a nice, normal young woman who would probably like to get back to the business of being able to pee and have sex freely, and he saw no reason why he couldn’t make that happen. He determined I no longer had an active infection—and then proposed a procedure, to be done right there, that day, in the office. As he described it, he would insert a small instrument into the urethra, rip it, and this would solve the problem.
I frowned.
At elegant cocktail parties, people were constantly cornering me to talk about their vaginas.
But Dr. Damaskus assured me it was the only option, should I want a normal life again—the gentle ripping, he explained, was more of a light stretching of the tissue, and it would interrupt the muscle spasm and break the cycle of pain. He handed me a paper gown.
I’m almost nostalgic for my naiveté. I took the gown, steeled my nerves, saddled up, and put my feet into the stirrups.
The procedure began benignly enough with a small swabbing of topical lidocaine, but in the next step, a device not unlike a very small car jack was inserted into the urethra and then ratcheted out several notches until the urethra, as promised, tore. It was a blinding pain that no amount of lidocaine would dull. He peeked over the paper blanket and asked if I thought he had gone enough notches. I was crying too hard to do anything but nod. He went one more notch.
Dear, patient reader, I have not forgotten about you or our purpose here—or the cautionary voice in the back of my head whispering something about too much information. But I think this history is important. So before we move out of this reverie, let me come quickly to the end of the beginning of our story.
That night, after Dr. Damaskus sent me hobbling back on my way, intuition’s warning bell finally took up its low, steady thrum. I sat silently through dinner and put myself to sleep early. Something was not right—something flu-like, but menacing, was starting to bristle. Everything hurt, not just my urethra. My ears hurt. My teeth hurt. I fell asleep, my hands clenching and unclenching of their own accord.
When I woke, I was on the floor, quaking with rigors, drenched in sweat, and making a very bad noise. My mother was calling the hospital and dragging me toward the car. I had become septic, with an infection of the bloodstream that would have ended badly if my mother weren’t such a top-notch physician. We were at the hospital in minutes.
I was not witness to the miraculous save, but I heard all about it when I woke up. Top-shelf, nuclear-grade antibiotics pumped into me by the gallon, and it seemed as if every doctor at Sibley Memorial Hospital came to sit by my side, making sure the doctors’ daughter pulled through. I was extremely well taken care of. I was going to live. It would all be all right.
By the next day, everyone had gone back to their private practices, wishing me well, which I very much appreciated. The only problem was (and I hated to be a stickler) I wasn’t all right. I was still aching all over, badly, even though the infection was gone. I had a fever every afternoon and intense pain all down my legs. The broken-glass pain was starting to radiate out to the surrounding muscles in the vagina, rectum, and bladder. My bowels seized up and stopped working. I itched.
“Strange,” my doctors murmured, making notes. “How very strange.”

They ran dozens of tests, but everything came back negative. At a loss (and at my insistence), they sent me back to school with painkillers and portable IV antibiotics. They said it would slowly all start to get better, and I believed them. When had my body ever done anything but get all better? I was ready to get back to the business of peeing and expressing my sexuality freely. I would carry my little IV from class to class if that’s what it took.
But my body did not get better.
Class after feverish class, night after achy night, and morning after urethrally excruciating morning, I could not deny: It was getting much worse.
And in the most mysterious ways.
I was on so many medications and getting so sick so fast, it was as if a rabbit hole had opened up beneath me—as if I were falling slowly past the clocks and the candlesticks, and my parents and doctors were peering over the edge, quietly watching me float down and away.
The entire point of The Lady’s Handbook for Her Mysterious Illness is this:
It would have been helpful to know what a well-trafficked rabbit hole that was.
The unfortunate but innocuous series of medical events.
The gallons of antibiotics and fistfuls of painkillers.
The severe digestive issues, gynecologic issues, joint pain, itching, and fatigue.
The referrals, the specialists, the puzzlement. The growing doctor/patient antipathy.
The dramatic health avalanche.
The clocks. The candlesticks.
The despair.
I thought I was the strangest medical case on the East Coast. I was wrong.
WOMI.
wo•mi | whoa-mee | noun
A woman with a mysterious illness.
I had to make this word up myself. I would have preferred a committee or a wealthy patron—whoever is in the business of naming—to do it for me, but no one volunteered. I’d also have preferred something more dignified than WOMI—something with gravity, preferably in the Latin. Something that provoked the right response, which in my case is “Holy f—ing shit.” But because there is no name for what’s wrong with me, people don’t say holy f—ing shit. They ask if I have tried green juice or positive thoughts.
Having a word helps.
And 17 years later, I have become a well-known WOMI.
In the early years of this distinction, other women with mysterious illnesses would frequently introduce themselves to me, often at the most unexpected moments—at weddings, in elevators, or leaning across a bank of guests at a crowded Thanksgiving table—all wanting to discuss their own mysterious maladies. I just had to speak the words candida or subclinical hypothyroidism—or the most potent of all, gluten—and three heads would rubber-band in my direction. They either knew a woman with a mysterious illness, were married to a woman with a mysterious illness, or were themselves a woman with a mysterious illness. While other people grilled kebabs, we would speak discreetly and in low tones about constipation. When the daiquiri pitcher appeared from the kitchen, we would duck our heads to discuss whether or not daiquiris were gluten-free. At elegant cocktail parties, women were constantly pulling me into corners to talk about their vaginas.
WOMI (n)
Her chronic, misunderstood, at times incapacitating ailments might include . . .
lupus
arthritis, fevers, fatigue, hair loss, sores, rashes, confusio
fibromyalgia
widespread, debilitating pain
sick-building syndrome
headaches, eye irritation, inability to concentrate, fatigue
chronic fatigue syndrome
incapacitating exhaustion, short-term memory dysfunction, joint pain
chronic lyme disease
fatigue, joint and muscle pain, brain fog
leaky gut
chronic diarrhea, constipation, bloating, brain fog, skin problems, sugar cravings
You most likely know one of us already—a coworker, an aunt, a sister—some beleaguered old girl endlessly dealing with her health issues.
She is exhausted, and likely in possession of at least one autoimmune disease. She is allergic to ____ (everything), aching from tip to toe, digestively impaired, and on uneasy terms with her reproductive system. She is addled, embarrassed, ashamed, and inflamed. She’ll be reluctant to talk about the particulars but noticeably lacking in a solid diagnosis. Most people privately agree she actually suffers from an acute case of hypochondria.
This woman may not know it yet, but she is in the club.
The following scene is unfolding in an office in your town every day, perhaps right at this very moment:
Jane Doe crosses her ankles in the waiting room, absently turning the pages of People magazine. She looks around often—now at the oversize clock, now at the receptionist, now at the generic watercolors on the walls.
“Ms. Doe,” a flat voice calls out. “Dr. Bowels will see you now. Second door on the left.”
Jane takes a seat in the doctor’s office and regards the diplomas on the wall. On the desk stands a life-size replica of the human intestinal tract. When Dr. Bowels bustles in, he introduces himself as he looks over her chart for what is clearly the first time.
“Now, Ms. Doe,” he says cheerfully. “What can I do for you?”
The interaction begins very seriously, a furious scribbling of notes, a furrowing of the brow, a lot of nodding. The usual diseases are ruled out, and Jane confirms she has been tested, twice, for everything under the sun. Her primary symptoms are severe constipation, distention, and pain in the lower left quadrant of her abdomen. As the doctor pages through her thick medical file, Jane takes the opportunity to share some of the stranger non-bowel symptoms she has experienced—aching in the bones, fatigue, itching, unexplained gynecologic symptoms, memory problems, lower back pain—but the words are scarcely out of her mouth before she wishes she had kept her addenda to herself. She can see the red flags rising behind his eyes, and the note-taking slowly tapers off. Before she knows it, where once Sherlock Holmes scribbled furiously, hot on the trail, bent on solving her mystery, he now leans back in his swivel chair, tip of his pen in the corner of his mouth, checking his watch. His look is saturated with understanding, for he has solved the case.

What we have here is not a rare, tropical disease, Watson. What we have here is an unhappy woman, badly in need of an antidepressant.
For years, I thought Jane Doe’s situation was unique to me. My own repeated disappointment at doctor after doctor, and all because my disease was either too weird or too unimportant. It wasn’t exactly chronic fatigue syndrome (a bit too gastric and much too pelvic), but it didn’t appear to be any of the known gastroenterological or gynecologic diseases, either. It was also monumentally more painful than anyone could explain. Repeated colonoscopies and biopsies revealed it wasn’t a known inflammatory-bowel disease like ulcerative colitis or Crohn’s.
Despite a truckload of symptoms, it appeared I had nothing at all.
And so maybe, because so many doctors seemed to quietly think so, it was hard not to start to think it was a simple matter of depression after all. How could they all be wrong? Never mind that antidepressants made me more depressed when I tried them. Never mind having built an all-around wholesome life despite my debilitating illness. And never mind my winning disposition and famously positive thoughts. If so many doctors were independently questioning my psychological composure, perhaps there was something to it.
I was just starting to believe this when I met my first WOMI. Her name was Charlotte.
We were brought together by our respective boyfriends at the time, and we sat for an afternoon at her small kitchen table. Piece by piece, she unfolded before me the patchwork story of her own mysterious illness. As I listened, I went absolutely pale, looking at her as I would at a secret twin, separated from me at birth, reunited at last. Her story was so familiar—eerily familiar. I had never heard myself described to myself before. The mortal exhaustion. The disaster in the pelvis. The distinct feeling of being 80 years old, despite being officially 25. I could not believe I had met someone so identically strange.
But then it wasn’t very long afterward that I met Naomi, a friend of my brother’s who regaled me with the story of her own mysterious illness over the telephone. A Silicon Valley mogul, Naomi had become sick with a virus when she was 32, immediately become bedridden, hidden away from society for years, unable to digest anything, allergic to most of her pantry, aching all over, and prescribed enough Valium to sedate a rhinoceros.

And as she spoke, I thought: Oh, my God. Secret triplets.
What incredible fortune that I would meet the only two others in the whole wide world forsaken with the same wretched curse.
But then, of course, I would soon come to meet Courtney and then Alexandra and Skye and Christina—followed by Gwen and then Greta and then Mara and then Jones—who all, to my ever-lessening surprise, recounted almost the exact same story as my own. Varying types of related-sounding illnesses and varying levels of severity—but undeniably variations on a very distinct theme—over and over again, almost the exact same story of the misdiagnoses, the medications, the disbelief, the rabbit hole, the Caterpillar, the Hatter, and the Hare.
And every single one of them thought she was the only one.
But she wasn’t.
They were all WOMIs.
And as we would all soon come to see—indeed, as you yourself may soon come to see—we were absolutely everywhere.
Excerpted from “The Lady’s Handbook for Her Mysterious Illness,” © 2020 by Sarah Ramey, published by Doubleday on March 17, 2020. The names in this story have been changed.
This article appears in the March 2020 issue of Washingtonian.