A week before seven-year-old Callum died, the scene in his family’s kitchen probably looked like this: An auburn-haired boy bounced around the room while his mother prepared his school lunch. His father downed some coffee before kissing his wife and hugging Callum, then headed to work. When her phone chirped that afternoon, Callum’s mother, Siobhan, knew something was wrong. Nobody called her at that time of day. Usually, calls started with “Callum is fine,” but the nurse didn’t say that.
A few days later, Callum was in a hospital bed at Johns Hopkins, choking on a breathing tube. His closed eyelids were small, taut balloons, his curls pasted to his skull. The ventilator wheezed as Siobhan and her husband, Rory, watched in disbelief.
When the EMTs had burst into the ER with the boy motionless on a stretcher, not breathing and volcanically hot, the doctors’ first thought was infection. A tube was plunged down Callum’s throat, needles jabbed into his elbows. I was the consulting physician called in to determine if the doctors’ hunch was right.
The parents were Irish, and Rory’s voice was memorable for its buoyancy, flying in the face of his crushed expression. When my colleagues and I walked into Callum’s room in the pediatric intensive-care unit, Rory stood with his hand outstretched while Siobhan tearfully looked up from her son and smiled. Their pleasant demeanor was unwavering.
The results of the blood culture popped up in less than an hour: rod-like bacteria. The precise definition was Gram-negative, non-lactose fermenting rods. Such bacteria shouldn’t be seen in a healthy child’s blood.
Most of our family meetings happened at bedside. Callum lay bloated from IV fluids, his parents leaning over him. His father’s five-o’clock shadow was way past midnight now, green eyes shocking against his ruddy complexion. Callum’s grandmother, who’d arrived from Ireland, stood by the wall, her hair disheveled, staring at us with those same eyes, the same soft smile.
I didn’t trust my own voice, even less so when I looked at Callum, so I kept my eyes on his family, this cluster of swollen love and heartbreak. I spoke slowly: Callum had meningitis, an inflammation of the lining of cells around the brain, due to an unusual infection, Pseudomonas aeruginosa. He also, we discovered, had an underlying condition—leukemia. As I explained this, I realized none of it mattered to these parents. There was nothing we could do for Callum. The infection had overwhelmed his brain, rendering it mute. There was no way to wake him or to encourage him to peer at us with his brilliant green irises. The family shared the same hair color, a soft cinnamon, akin to the cookies Callum’s grandmother had brought for the medical team.
At a time like this, doctors’ words are rehearsed, used time and again with slight changes. “We’ve done all that we can. Callum’s disease has devastated his brain. We don’t see much of any cerebral activity. His body has shut down. We’re keeping him alive with our machines. We’re so sorry.”
It’s almost too simple to say goodbye to a child like Callum. A parent expects the world to take notice. But things were different with this family. Although they were in intense pain, they accepted his fate and, incomprehensibly, seemed at peace.
Their gratitude for the little we’d done for their boy was haunting. So was the thought that people in the world had no idea a second-grader named Callum had been born, fed, loved, disciplined, coddled, sent to school, and then had died. Each young patient is a person who means the entire world to a family, whose lives fracture when that child dies. We physicians have the privilege and, arguably, the misfortune to view the shuttering of a life in such starkness, in such light, and with such clarity.
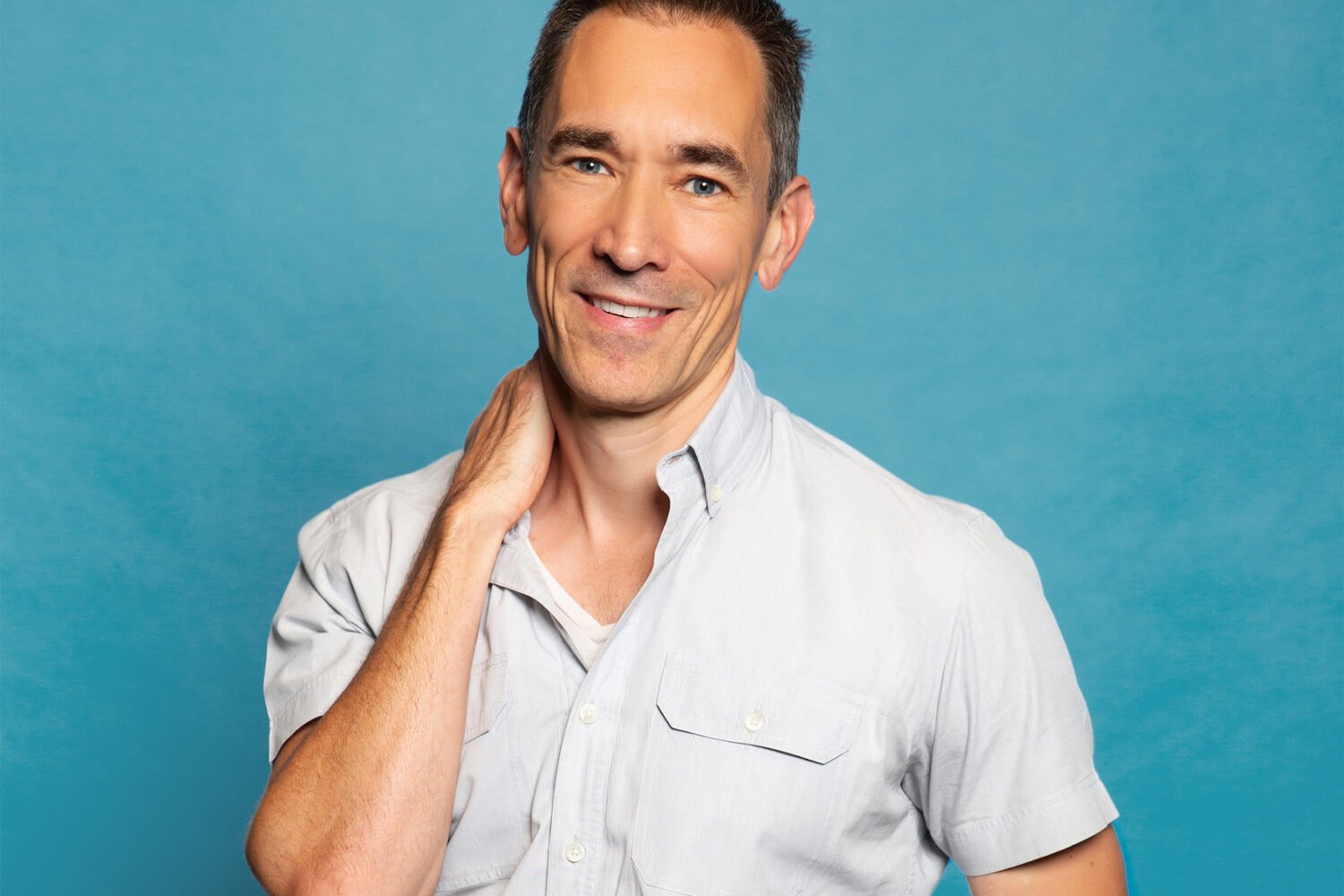
Tafadzwa Kasambira (tkasambira@gmail.com) is a pediatric infectious-diseases physician living in Silver Spring. On Twitter, he’s @drkasambira.
This article appears in our August 2016 issue of Washingtonian.