In a dimly lit exam room, a sonographer at the University of Maryland Medical Center’s Center for Advanced Fetal Care points to a bright spot.
“See this right here?” she asks. “This baby’s intestines look a little brighter than the other ones.” The discrepancy could be nothing, she says. It could also be a marker for Down syndrome or cystic fibrosis.
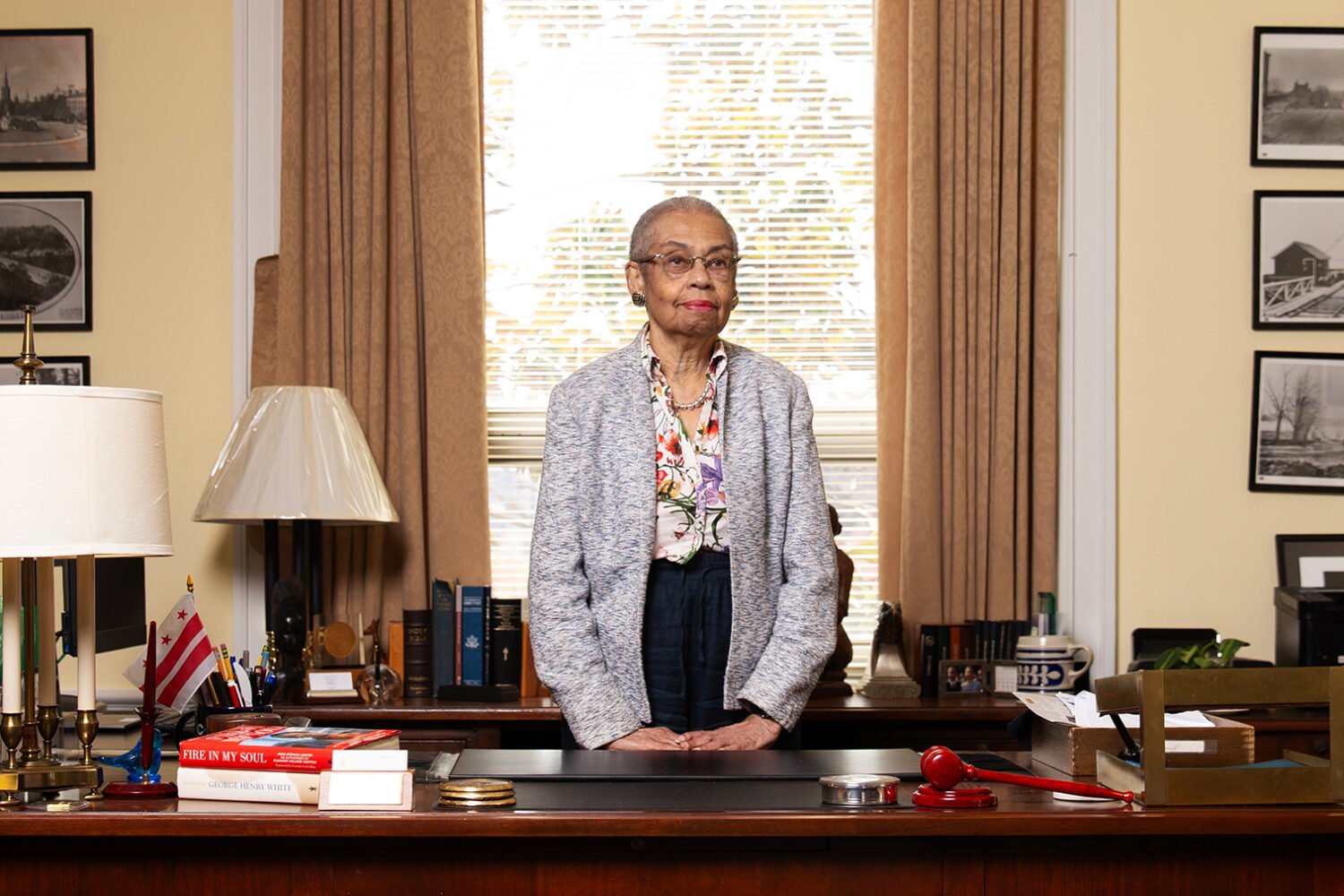
Kathy Powers stares at the screen. Naturally calm and optimistic, she has faith in the results from the amniocentesis, which showed that all three of the babies were healthy. But she’s already worrying about how she’ll relay the news to the babies’ biological mother, whom she’ll call the moment she leaves the appointment.
As the sonographer prints out images of the ultrasound, Powers, a mother of two from Odenton, wipes the warm gel from her stomach and hikes down her shirt. She glances at the quartz bracelet she made three pregnancies ago; a silver bead on it reads believe in miracles. She made an identical bracelet for Kim Crane, the Virginia woman to whom she’ll send the photos.
Powers does believe in miracles. She has believed in them since she conceived her own children with help from fertility treatments, and since seeing Crane’s tears of joy after Powers gave birth to Crane’s son in 2006. “When you share that experience with someone else, it’s the most amazing feeling, to see them holding their own biological child that they could not have on their own. To think I did that!” Powers says. “I knew right away, in the delivery room, that I wanted to do it again.”
Now Powers is on her fourth pregnancy as a surrogate and her sixth overall. She is 48 years old and 18 weeks pregnant with triplets that aren’t hers. Two of Crane’s embryos implanted in Powers’s uterus, and one split into identical twins, a situation so fraught with risk that a local fertility specialist calls Powers a “ticking time bomb.”
Before she began in vitro fertilization, or IVF, Powers and the intended parents discussed what would happen if there were a problem with the pregnancy. All preferred to do everything they could to save the baby, or babies. Once they learned that Powers was carrying triplets, however, they decided to follow doctors’ orders. Three of the four physicians they visited said the pregnancy should continue. The fourth disagreed, but Powers and the parents dismissed his concerns as “doom and gloom.”
Now Powers holds fast to her belief that everything will be all right: “I choose to think positive and believe they are strong little miracles and nothing bad is going to happen to them.”
• • •
In deciding to become a surrogate, Powers joined a small but growing contingent of women. Nationwide, the number of gestational surrogate births rose by 122 percent between 2004 and 2011, from 530 to 1,179, according to the American Society for Reproductive Medicine.
DC is the only jurisdiction in the country in which all surrogacy contracts are prohibited. Any party involved can be imprisoned for up to a year and fined as much as $10,000. Maryland has no statutes or limitations governing gestational surrogacy and has become one of the world’s hot spots for surrogacy. Virginia is another relatively surrogacy-friendly state.
For would-be parents—especially couples with fertility problems, gay couples, and single dads—surrogacy’s appeal has grown as both domestic and international adoptions have become harder.
There was a 122% increase in the number of gestational surrogate births nationally between 2004 and 2011.
But the reasons women decide to carry someone else’s child are less obvious, especially when they do it for a stranger. Who would endure the morning sickness, weight gain, out-of-control hormones, and constant doctors’ appointments—not to mention labor—without the payoff of a new baby at the end? For a mere $20,000 to $30,000?
The answer, in part, is women who love being pregnant, suffer few of the unpleasant side effects, and even enjoy giving birth.
The idea of becoming a surrogate occurred to Kathy Powers after she turned 40 and told her husband she wanted another baby. He wasn’t receptive—another child would mean spending money on fertility treatments, risking the birth defects more frequent with older mothers, and managing a new college fund when they already had two great kids. He didn’t want to tempt fate.
After some soul-searching, Powers realized that she craved pregnancy, not another child. With no morning sickness and with easy deliveries, her pregnancies had been dreamy. “My hormones are perfectly, 100 percent in line with the universe when I’m pregnant,” she says. “I’m the happiest I ever can be in life.”
So she presented her husband with a compromise: Instead of having a baby of their own, she would carry one for someone else. They’d had difficulty conceiving their second child, and they decided that she would be a surrogate only for someone who had struggled as they had. “I didn’t want to be pregnant for a movie star who didn’t want to be fat,” Powers says. “It had to be someone we could relate to, who we really feel like we’re helping, because we’ve been there.”
She placed an ad on three surrogacy websites, received 30 replies within two days, and felt an immediate connection with Crane and her husband, who already had one adopted child. “It was one of those meant-to-be things,” Powers says. “We agreed on every term.” Three months after they met, a reproductive endocrinologist transferred Crane and her husband’s embryos.
After Powers gave birth to the couple’s baby boy in 2006, the endocrinologist gave her phone number to another Virginia couple interested in surrogacy; in 2008, she delivered their first child, and two years later their second.
By then, Powers figured she was done. But when Kim Crane asked her to help find a surrogate for her leftover embryos, which had been frozen for 6½ years, she offered to come out of retirement. She felt a responsibility to the couple and couldn’t imagine someone else completing their family.
The second embryo transfer was successful, but joy turned into shock when the five-week ultrasound showed three heartbeats. For the first time in her life, Powers hasn’t had an easy pregnancy—suffering through nausea, bleeding, and exhaustion. She has already been restricted to some bed rest and been told to expect more.
“And then,” she says, “there’s the emotional part.”

The emotional part. It’s probably not what you’re imagining.
One of the most common questions surrogates hear is “How will you be able to give up the baby?” But when surrogates talk about the “bond” they form, they’re usually referring to one with the intended parents, not with the baby. They may not imagine what the infant will look like, or rub their belly as they did when pregnant with their own kids.
“I sometimes forget I’m pregnant until someone asks when I’m due,” says Julie, 37, who lives in Silver Spring and recently had her fourth surrogate baby. (A confidentiality clause in her contract prohibits her from publicizing her last name.) “With your own child, you never forget; it’s like, ‘I’m 24 weeks!’ ”
Susan Fuller, a 44-year-old nonprofit director and fitness instructor in Reston, is pregnant with her ninth surrogate baby. She says that when people ask whether she misses the child afterward, she laughs. “The absolute last thing I want in my life is a baby,” she says. “I have three teenagers, and I’m thoroughly enjoying this phase of life. I still yearn for pregnancy and birth, but I don’t yearn for the baby.”
Fuller has had great experiences with most of her surrogate pregnancies. But the one relationship that didn’t work out, her first surrogacy, in 2002, remains a heartbreak.
Fuller’s first set of intended parents treated the situation more like a rent-a-womb transaction than the close relationship she’d hoped for. Because she was carrying twins, they wanted her to gain more weight and see a nutritionist, even though Fuller’s obstetrician said her pregnancy was going well. When Fuller refused, the father broke off contact with her.
Worse, the birth was traumatic: Fuller delivered one twin vaginally and the other by emergency C-section, lost a lot of blood, and was in the hospital for five days. The new parents were distant, and the mother visited her only once. Fuller was devastated.
Six months after the delivery, she called the surrogacy agency that had matched her with the couple and asked to do it again. “Oh, my God—after everything you went through?” the agency head asked her.
“I want my love story,” Fuller said.
When asked what that meant, Fuller doesn’t mention the babies. She describes a relationship “where you both grow to love each other, to be excited to complete or add to their family. Because you want them to experience the joy of parenthood and you feel the support and the gratitude from them. It’s this homeostasis of ‘I can’t believe you’re doing this for me’ and ‘Oh, my God—it makes me so happy to do this for you.’ ”
$23,000 is the typical fee for a first-time surrogate (experienced surrogates and those carrying multiples are paid more).
Fuller has since found her love story several times over. With the exception of one stillbirth at six months because of a heart defect, her pregnancies have been blissful, her deliveries easy, and her relationships fulfilling.
Many fertility centers and surrogacy agencies will use only surrogates who have had fewer than five deliveries or three C-sections. Not all agencies are regulated, however, and people who make matches independently on websites don’t necessarily adhere to the medical recommendations. Some women have done as many as 10 or 12 surrogacies.
Fuller is now carrying her 12th baby, but she says she’s not worried, because both her obstetrician and her fertility center have cleared her before each pregnancy. She’s never had high blood pressure or high blood sugar, and she teaches exercise classes up until she goes into labor. During her last pregnancy, she took a kickboxing class the evening before her due date—and delivered ten hours later. She figures she’s not only fit to carry but also more thoroughly tested than the average mother-to-be. Plus, she says she truly enjoys “the endorphin rush of pushing a kid out”—she has given birth to five babies without drugs.
After the births, Fuller is content with occasional photos and e-mails, and only rare phone calls and visits, to learn how the babies are doing. “You’re interested and care about them,” she says, “but as someone else’s children, not your own.”
• • •
And the fact that these are someone else’s children brings a certain pressure.
Twenty years ago, before IVF became mainstream, “traditional surrogacy” was the norm. A surrogate was both the egg donor and the carrier, inseminated with sperm from the intended father. Now the vast majority of surrogates are “gestational.” They have no biological tie to the baby because the egg comes from the intended mother or a donor.
This shift means the surrogates must endure IVF, an invasive process that can involve painful testing, up to 16 weeks of hormones delivered by injections or pills, an embryo transfer, and blood tests—procedures repeated for each attempt.
The two-week wait between the embryo transfer and the pregnancy blood test can be “horrific” for a surrogate, says Pam Stepka, an Ohio surrogate who twice has carried babies for a Washington couple. About three days after each transfer, Stepka bought 30 pregnancy tests and started testing two or three times a day. “When I was pregnant with my own kids, I took one test and was like, ‘Oh, I’m going to have a baby,’ ” she says. “I never thought it wouldn’t stick. Not so with this. You see that faint line and you’re taking the test apart, holding it up to light and asking your husband, ‘Do you see? Is that a little bit different?’ And then you continue testing because you want that line to get darker. ”
Stepka dreaded telling the intended parents when her tests were negative. “It felt like it was up to me. It’s so hard to have to say, ‘No, nothing yet,’ when you know they’re waiting every day, wanting to know. But once you see that line, you’re ecstatic.”
At the same time, she says, throughout the surrogacies “I was so much more conscious that things could go wrong. I never felt like that with my kids. Every day you just feel 100 percent responsible for somebody else’s child.”

There’s a moment all surrogates remember. It doesn’t get old. It’s life-changing every time. And it’s so powerful that every surrogate interviewed for this article had difficulty capturing the experience in words.
When the baby is born, the awe, joy, and gratitude in the delivery room are nearly as breathtaking for the surrogate as they are for the new parents. “When you see the incredible miracle that happens when they look at their baby,” Powers says, “there’s nothing like that feeling except having your own baby.”
Surrogates repeat the process for many reasons—because of the way it makes the parents feel, because of the way it makes them feel, because they can. “I don’t like the idea of my uterus just sitting around doing nothing when there are others who would give anything for what has been given to me,” says Beth Anderson, an Eastern Shore labor-and-delivery nurse embarking on her second surrogacy. “How can you not share that?”
Anderson, a mother of two, delivered a baby to a Virginia couple in 2012. She was inspired to become a surrogate after seeing patients with second- and third-trimester fetal loss. “Seeing the same people coming in with repeat losses is heartbreaking,” Anderson, 32, says. “And it is so wonderful to see those people finally get the baby they have been trying so hard for.”
Julie, the Silver Spring surrogate, says: “My single proudest moment was doing what I’ve done for those people. It was the most important thing I will ever do in my life.”
• • •
Allison Wylam, 36, is feeling warm and fuzzy as she drives home from a match meeting.
After her third surrogate delivery in November 2011, Wylam thought she was finished. She had given birth to four kids of her own and three others for three couples, all without drugs. For each of her surrogacies, the doctor broke her water and she gave birth within 30 or 40 minutes.
But seven pregnancies was a lot.
Over the last few weeks, though, Wylam has felt “a strange pull to do this again,” she says. Three weeks ago, Meryl Rosenberg, an attorney who runs a surrogacy program in Potomac, called her to check in. When Rosenberg joked about a fourth surrogacy, Wylam said, “Actually, that’s been on my mind.” Rosenberg told her about a new couple, and Wylam agreed to a meeting. Wylam’s doctor gave her the green light for another pregnancy should she want one.
She does. “They’re a really good couple, very excited, very inquisitive,” Wylam says, still giddy from the meeting. “They both had smiles on their faces the whole time.”
It took only about 20 minutes for Wylam to know she wanted to carry a baby for these strangers. The decision has always been easy for her. Her first set of parents had miscarried at 20 weeks, and their heart-wrenching story convinced Wylam to become a surrogate. Now, after listening to her fourth couple describe their difficulty finding an experienced surrogate, she knows she’ll help them start their family.
Before the “match meeting”—the initial consultation during which the intended parents and the surrogate gauge their compatibility—the agency has already conducted a background check and, usually, an in-home interview.
“We’ll talk to the mother, best friend, someone she’s worked for,” says Diane Hinson, the founder of Creative Family Connections, a Chevy Chase law firm specializing in surrogacy. “It’s an intense prescreening process. We probably go through more than 30 women just to find one to interview.”
Rosenberg says one of the most crucial issues parents and surrogate need to discuss is their philosophies about selective reduction and termination: How do they feel about triplets or genetic problems?
Although contracts spell out their agreements, they’re not necessarily enforceable. “My job is to worry about the what-ifs,” Rosenberg says. “No court will ever order a gestational surrogate to terminate or reduce. The reason we talk about this over and over is we never want to be in a situation where people are on two sides of the fence.”
That’s where situations can get dicey. In 2012, for example, a Connecticut couple using a surrogate learned at five months that their baby had brain abnormalities and serious heart defects. The intended parents offered the surrogate $10,000 to have an abortion. She refused and moved to Michigan, which recognized her as the child’s mother. She found the girl an adoptive family there.
• • •
Contracts can also veer into specifics: avoiding sushi, limiting caffeine, refraining from extreme activities such as skydiving.
“More times than not, a surrogate will say, ‘Is there anything special you’re looking for me to do?’ ” Rosenberg says. “Most surrogates I deal with really work hard to take even better care of themselves than when they had their own children.”
Rosenberg has represented intended parents who asked their surrogate to eat only organic foods. (The parents reimbursed grocery costs.) Another client asked Rosenberg whether a surrogate would keep kosher. Rosenberg suggested instead that the surrogate avoid seafood and pork. Jennifer Fairfax, a Silver Spring family-law attorney, has seen contracts stipulating that the surrogate not have hair treatments, because of the chemicals, and requested that she avoid all places that use hair-treatment products. Another couple asked a meat-eating surrogate to become vegetarian during the pregnancy.
One of the most important contractual restrictions is a clause that prohibits out-of-state travel in the third trimester so that a surrogate doesn’t deliver in an unfriendly jurisdiction. Nobody wants a Maryland surrogate to deliver in DC. Several years ago, another attorney asked Fairfax for advice on a case in which a surrogate accidentally gave birth in DC, which doesn’t recognize a parentage order from another state. “The carrier ended up on the birth certificate, and it ended up being an adoption,” Fairfax says.
This situation may change within the year. In June, the DC Council Committee on Judiciary and Public Safety held a hearing on a bill introduced by Councilman David Catania. The Surrogacy Parenting Agreement Act of 2013, which would legalize and provide safeguards for surrogacy contracts in the District, is cosponsored by every other member of the council.

The office of Creative Family Connections, a large suite in the Chevy Chase Metro building, doesn’t look like the first stop on a baby-making journey. No photographs of laughing babies line the walls; no serenely pregnant surrogates rest their hands on their bellies in the waiting room.
By the time clients come here, many of them have been through a lot, struggling through fertility problems and miscarriages. “We have people come in and cry, which makes us cry,” says Diane Hinson, who founded the firm. “One of the worst was a couple, and the wife, with tears streaming down her face, was sitting right there”—Hinson gestures to the conference-room chair across from her—“telling us how they had been through an entire adoption process after three or four unsuccessful IVFs, and then three days after they got the baby, the birth mother changed her mind and took the baby out of her arms.” Sixteen months later, the couple’s surrogate, whom Hinson selected, delivered twins.
Hinson told the couple, as she tells every client, “We are 100 percent successful at matching people, and everybody who sticks with the medical protocol and advice goes home with a baby. ”
The minute clients hear that, she says, their shoulders relax and their tears dry: “They’re like, ‘Really?’ I’m like, ‘Really!’ That’s our history. That’s why we reject so many surrogates. We want the cream of the crop.”
• • •
Hinson was inspired to start her company after asking some of her gay friends what they did when they wanted to start a family. They told her they went to California, where there were more established surrogacy programs. “I said, ‘Well, that’s insane—you shouldn’t have to go to California.’ ”
Surrogacy has become more common among gay and lesbian couples partly because international adoption is mostly closed to people who are out of the closet.
Robert, a prominent anesthesiologist, says that for decades he didn’t think that as a gay man he could become a parent, though he always held out hope. Then he and his husband, Jeffrey (both identified here by their middle names), attended an eight-week seminar called “Maybe Baby” led by Ellen Kahn, president of Rainbow Families DC, a support-and-education organization for LGBT-headed households.
Robert and Jeffrey signed up with an agency, and within a month they met their surrogate and hit it off. She got pregnant with the first transfer but miscarried after 13 weeks. “It was heartbreaking,” Robert says. “It’s also a race against the clock with money, because every attempt is thousands of dollars. It’s not like there’s an unlimited number of tries to do this, because at some point the money’s going to run out.”
When their daughter was born, Robert says, “I remember calling my mom and telling her and there was a sense of almost, ‘Wow, I’m normal, too.’ For someone who grows up thinking they’d like to be a dad, it seemed for so long like a dream that didn’t seem possible. I remember feeling complete.”
Today, Robert and Jeffrey live in a “wonderful, crazy” Northwest DC household with their three-year-old daughter and two-year-old twin sons, carried by the same surrogate.
They remain close to the surrogate, who has visited several times and sends the kids birthday and holiday gifts. “We consider her a part of the family,” Robert says. “It’s something that she’s given us three times that we can never repay her for. We hope that she’ll be in our lives for the rest of our lives. Someday we’ll invite her to graduations from high school and college and—” here he breaks down—“I hope she’d be as proud as we are.”
• • •
Surrogates say their relationships with mothers-to-be can be more complicated than with the dads. While women are grateful to the surrogate, they also might grapple with mixed feelings if they mourn the inability to carry their own baby.
Sandra Lippard, who lives in Bethesda, turned to surrogacy at age 41. As a self-professed type A, she found it difficult to watch someone else carry her child. “In the beginning, you feel like you’re in the driver’s seat because you’re paying all this money,” she says. “But then she’s pregnant with your baby and you cater to her.”
Lippard first realized she couldn’t control the situation when she and her husband drove out of the fertility clinic’s parking lot. In her rearview mirror, she saw the surrogate—who was carrying their twins—listening to her iPod on earbuds as she drove back to Pennsylvania. Lippard worried that the surrogate would get into an accident, and her husband had to calm her down.
The surrogate’s own husband wasn’t as supportive. When the surrogate had to go on bed rest, her husband refused to let Lippard hire a maid service; a surrogate’s contract typically includes provisions for child care, lost wages, and maid service if she’s confined to bed. “He put down his foot and said, ‘No, I’m not going to have someone else pay to take care of my family.’ Meanwhile his wife—an angel who goes out of her way for everybody—was on the couch feeling guilty,” Lippard says. “I got on the phone with him, and he tried to call my bluff, saying, ‘Why don’t you come out here and clean the house for us?’ And you know what? I said, ‘Okay, I’ll be there tomorrow.’ I lived at their house for three weeks. I cleaned their house, did their dishes, did their laundry, changed their one- and three-year-olds’ diapers, and cooked dinner.” A few years later, Lippard started her own small surrogacy agency.
Surrogates’ husbands can be caught in an awkward situation. They won’t be able to have sex with their wife while she’s going through IVF, and they need to be willing to help out if she’s on bed rest. Some use humor to deflect the strangeness of the circumstances. “My husband thought it was funny to say his wife was pregnant but it wasn’t his,” Stepka says. “He’d let that go for a minute or two and then say, ‘Yeah, she’s carrying for a friend of ours.’ ”
Doug Fuller, Susan’s husband, admits that in the beginning he was concerned about how another pregnancy would affect their sex life, not to mention the usual health risks. But he agreed to the surrogacies because, he says, “I could see how important being a surrogate was to her and I didn’t think I could live with myself if I was the impediment to her doing it.”
When Kathy Powers became a surrogate the first time, she introduced her kids, then eight and four years old, to the intended parents. She told them the mother’s “tummy was broken and I was going to help her have a baby.”
Powers felt it was crucial for her children to know where the baby was going—“for them to know I didn’t just have this baby and give it away. They held the babies; they saw the intended parents take them home. We’re extended family at this point. My kids are like cousins with them.”
Her daughter, Carianne Powers, now 16, says she wasn’t much affected by her mother’s surrogacy until she was a freshman in high school. When she did a biology project about IVF babies, her mother came in to talk to her class.
“All my peers were silent. Then they were like, ‘I’ve never heard of this before, and it’s the strangest thing ever,’ ” Carianne says. “I couldn’t talk to them without them thinking, ‘Oh, her mom is the very strange pregnant woman.’ ” But as Carianne’s close friends got to know her mother outside of class, they came to see surrogacy as less weird.
Carianne says her mother always talked with the whole family before signing on to be a surrogate. “It was only weird when people would see us together, like when we went out for frozen yogurt and a lady said, ‘You must be excited for all of these siblings!’ ” Carianne says. “I just said, ‘Yep.’ But if it’s someone we’re going to see more than once, then I have to explain and it takes a long time, or they get the wrong perception of it. And they keep thinking, ‘What is up with that woman?’ ”
Kathy’s husband, James, says that when she brought up the idea of surrogacy, his first reactions were “(A) There is never a dull moment with this woman and (B) what a wonderful thing to do.”
Like Doug Fuller, he worried about the health risks but agreed to the surrogacies “because I love my wife with all my heart and soul and want nothing more than for her to be happy. But also to give back. The idea of giving someone else the sense of joy my children give me was just overwhelming.”
After Kathy’s second surrogacy, she and James spent a few days in the hospital with the new parents and their baby. James recalls a scene from that time that he’ll never forget. The baby was buckled into the car seat. “The only thing left was to say goodbye before they drove one way with their new family and we drove home to ours. In that one perfect moment, words didn’t exist. I can’t begin to describe it, their reaction. It was an experience few will ever know.”
• • •
On a sunny afternoon in May when Powers arrives in Virginia for her second visit since the triplets’ birth, the babies are napping. For a few minutes, she stands next to Kim Crane in the nursery, watching them slumber. The triplets—two boys and a girl—were born at 32 weeks, two days gestation, with no health problems. The spot visible on the ultrasound disappeared after a few weeks.
Now nearly seven months old, they’re happy, snuggly babies, sturdy enough to hold happy mother’s day signs for a photo that Crane texted to Powers. Because Powers has driven more than an hour, Crane wakes the triplets so that Powers can interact with them. She helps Crane change and feed them and tears up when they smile at her. Crane takes pictures of Powers holding all three on her lap. Powers will later post the photos as her Facebook profile picture.
“To see them growing and thriving, it just warms my heart,” Powers says. “I feel so attached to them, and holding them feels different to me than the other babies. I don’t love the other kids any less—it’s just a different bond that I have with the triplets, I think because of everything we went through.”
Powers was on bed rest in the hospital for two weeks before her emergency C-section and was rehospitalized afterward with postpartum preeclampsia. She pumped breast milk for the babies for months, which she thinks further delayed her emotional and physical recovery.
Powers doesn’t mind. While she was on bed rest, Crane told her the names she had chosen. Her daughter’s middle name would be Katherine, after Powers. “She wouldn’t be here if it weren’t for you,” Crane told her.
Powers cried so hard she couldn’t speak. “I was overcome with joy, I was just so touched,” she says. “You never expect that.”
Alexandra Robbins is the author of six books. Ali Eaves is a former editorial intern.
This article appears in the September 2013 issue of The Washingtonian.