On the day he took his own life, Austin Trenum ate cheesecake.
He was 17. He loved cheesecake. He loved the Beastie Boys, too, and
SpongeBob Squarepants and the silly fauxhawk haircut he spent months
cultivating and two minutes shaving off because, well, that’s what
teenagers do. He loved his little Geo Metro convertible, neon yellow and
as macho as a golf cart, a gift from his grandfather, the two driving all
the way from Texas to Austin’s home in Nokesville, Virginia, a close-knit
community of 1,354 in Prince William County.
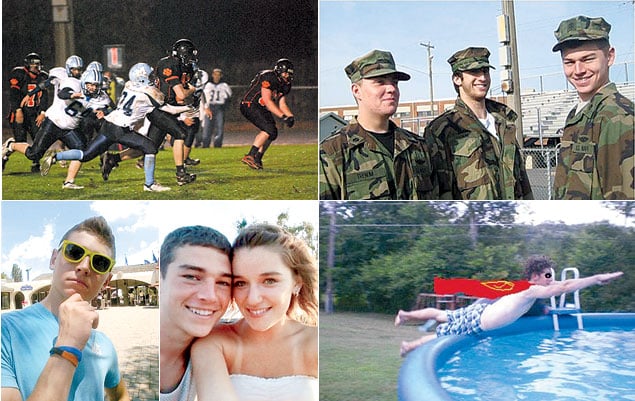
Austin loved his parents, Gil and Michelle, and his younger
brothers, Cody and Walker. He loved his girlfriend, Lauren. He loved
cheering for the girls’ volleyball team at Brentsville District High
School, smearing his chest with paint and screaming his lungs out
alongside his lacrosse teammates; loved sneaking out of his chemistry
class to sing “Bohemian Rhapsody” with his friend Carmen in the band room;
loved fishing and paintball, roller coasters and blasting “Sweet Caroline”
with the top down.
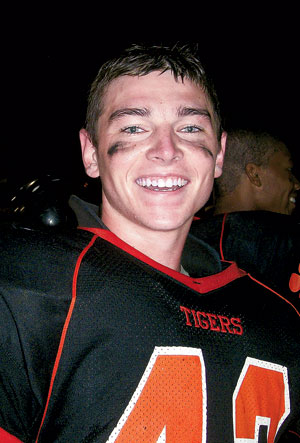
He especially loved football. Loved watching the Dallas
Cowboys. Loved playing for the Brentsville varsity team—fullback and
linebacker—taking hits and delivering them, seldom leaving the field,
eating two Hostess cherry pies before every game. He was a handsome kid,
green-eyed like his mother, six feet tall and 190 pounds, growing stronger
and more confident all the time. Under the Friday-night lights, in his
beat-up helmet and shoulder pads, you could see the man Gilbert Allen
Austin Trenum III was becoming.
• • •
It was Sunday, September 26, 2010. Michelle Trenum woke up
around 8 am. Gil was out of town, returning that afternoon from a weekend
drill with his Navy Reserve unit in New Jersey. Walker, ten, their
youngest, was on the living-room couch, hiding under a blanket. He jumped
up when Michelle walked in. Boo!
“Austin’s awake,” Walker said. “He’s in the basement playing a
video game.”
That’s odd, Michelle thought. Austin never got up early on
Sundays. Not voluntarily.
Michelle made her sons breakfast. Austin drove his other
brother, Cody, 15, to a lacrosse game and cheered from the sidelines. He
took more pride in his siblings than himself; he was that kind of brother.
On the way home, he teased Cody. “You did good,” Austin said, before
delivering the punch line. “You surprised me!”
Back at the house, Austin ate lunch. And cheesecake. While
Austin surfed the Internet, he and Michelle talked about Adam James, a
Texas Tech football player who had allegedly been locked in a dark
electrical closet by the school’s head coach, Mike Leach, after suffering
a concussion. The story, which ultimately ignited a media firestorm and
led to Leach’s firing, began when the injured James showed up to practice
in sunglasses and street clothes; Austin joked with his mother that he
should do the same, just to see how his high-school coach, Dean Reedy,
would react.
Austin then turned serious, balancing on one foot to mimic a
neurological test.
“Am I going to be out all week?” he said. “I don’t want to be
out all week. Do you think I’ll be out two weeks?”
“You’ll just have to see,” Michelle said.
During a football game the previous Friday night, Austin had
sustained a concussion. Brain trauma had been in the news. There were
reports of retired NFL players suffering from depression and dementia
linked to their hard-hitting careers. There were congressional hearings,
some of them dealing with high-school football. In the coming months, the
sport would be engulfed in a full-blown health crisis. Austin’s parents
were mostly unaware of the controversy. They had both grown up in Texas,
where football was king, where getting your bell rung was just a part of
the game. Almost a badge of honor.
• • •
Gil and Michelle had been in the Brentsville High bleachers on
Friday night, chatting with friends, a full moon overhead. Neither of them
saw the hit, but Gil spotted their son standing with his helmet off,
touching his index finger to his nose at the direction of team trainer
Richard Scavongelli. Just like last season. Good grief.
On the sideline, Austin was dazed, slurring his words. During
the drive to the emergency room, he was alert enough to call Lauren, his
girlfriend. By the time he was standing in line at Prince William
Hospital, shirtless and sweaty, he seemed fine. He cracked jokes, flirted
with the nurses who brought him a sandwich and a soda. He begged a doctor
to let him leave, asked if Lauren could come back to the examination
room.
A nurse asked if he wanted Tylenol.
“The last time you got a concussion, you got a headache,”
Michelle said. “Are you sure you don’t want it?”
“Mom, I’m fine,” Austin said. “I don’t have a headache. Except
for my normal football headache. I get them after every game.”
The medical staff gave Gil and Michelle a sheet of
instructions: Watch for vomiting and clear fluid coming out of Austin’s
nose, signs of a more severe brain injury. Limit their son to “quiet
activities” for the next 24 hours. Wake him from sleep every few hours to
check for evidence of intracranial bleeding, such as confusion and extreme
drowsiness.
Heading home, the Trenums stopped at the Chuck Wagon, a
restaurant around the corner from their house, where the Brentsville High
players gathered after games. Austin’s teammates recounted his sideline
exchange with Scavongelli.
Scavongelli: “Do you know where you are?”
Austin: “Yeah. This is my field!”
Scavongelli: “No. Do you know what school you are
at?”
Austin: “Yeah. My school!”
Scavongelli: “Do you know who you’re playing
against?”
Austin: “No.”

This is my field! Everyone laughed. They laughed at the way
Austin had gotten emotional on the field, too, cussing out one of his
buddies, something he never, ever did.
On Saturday morning, Austin attended football film study; that
afternoon, he went fishing; in the evening, he took Lauren to a Sugarland
concert, a belated celebration of her birthday. They sat on the Jiffy Lube
Live lawn, taking pictures under the stars. When Austin got home, he
texted Lauren good night. The next day, he was sitting in his family’s
dining room doing homework, texting her again about meeting up two hours
later to watch a Redskins game.
Austin was a good student, ranking in the top 6 percent of his
class. He planned to study chemical engineering in college and was
deciding between Virginia Tech and James Madison. The former had a better
football team; the latter, he deduced during a campus visit, had
better-looking girls. As Austin studied for his Cold War history class,
Michelle went online to check his academic progress. There was a problem.
He hadn’t turned in two papers. Michelle was upset and lectured him about
slacking off.
Gil came home around 2:30 pm. Michelle gave her husband a kiss
and cut him a slice of cheesecake. She told him about Austin’s schoolwork.
Austin looked irritated—almost angry. That was out of character. Michelle
saw his jaw clench. His mouth moved. She was stunned. Did he just call
me a name? Austin stared straight ahead.
“If you don’t finish your work,” she said, “you can’t see
Lauren tonight.”
Gil and Michelle went outside. Cody and Walker were on the
living-room couch, watching a football game. At some point, Austin went
upstairs.
“I don’t know what’s wrong with Austin,” Michelle said. “He
shouldn’t disrespect me like that.”
“He’s a teenager,” Gil said. “I’ll go talk to him.”
Gil went inside. He passed the kitchen table, where his
cheesecake sat untouched. He walked up the stairs, the same stairs where
Austin would ambush Walker when he came home from school, peppering him
with foam darts from a toy gun. The door to Austin’s room was
open.
Michelle Trenum heard her husband scream.
• • •
On her way to the hospital, Patti McKay made a deal with God.
Not Austin. Please. Take me instead. The boy was like a second
son. Every summer, the McKay and Trenum families vacationed together at a
lake in Maine, where the kids would play King of the Dock—wrestling for
control of a wooden swimming platform, tossing one another in the water,
Austin always making sure the younger children won their
share.
When her cell phone rang, Patti was in her sister’s garden,
kneeling in the dirt. It was Cody, panicked. Austin wasn’t breathing. Gil
was trying to resuscitate him. An ambulance was on the way. What should
they do?
Keep performing CPR, Patti said.
A cardiology nurse, Patti suspected a subdural hematoma. A
brain bleed. Which was odd. She had just seen Austin, about 90 minutes
earlier, pulling up in her driveway—the top down on his little yellow
convertible, Cody in the passenger seat.
Austin had been grinning. He had a gift with him, a Snickers
cheesecake.
“Here, Ms. McKay,” he said. “Look what we brought for
you.”
“How are you feeling?”
“Okay.”
“No, really—how are you feeling?”
“I’m fine. My headache is almost gone.”
Patti had been at the game on Friday night, standing with
Austin in the Brentsville High parking lot, holding his arm to help him
balance. But today his gait was normal, his hands weren’t shaking. She
called the emergency room, professional instincts taking over. You’re
getting a boy who had a concussion two days ago. You need a neurosurgeon.
If you don’t have one, have a helicopter ready to evacuate. Arriving
at Prince William Hospital, she didn’t see a helicopter. She saw Rob
Place, the Trenums’ next-door neighbor.
Austin hanged himself, Place said.
• • •
Nothing made sense. Not suicide. Not Austin. Not the boy who
went deer hunting in West Virginia with his father and crafted elaborate
zombie-apocalypse defense plans with Walker. Not the young man who always
said “Yes, sir” and “No, ma’am” and was adored by his friends’ parents.
Not the charmed kid who never got mad on the lacrosse field, who’d scored
a goal six seconds into his first high-school game.
“If someone came to me and asked me to rank, 1 to 25, the kids
on the team most likely to have problems and the kids who were the most
stable, Austin was number one on the stable end of the list,” says Carl
Kielbasa, Austin and Cody’s former high-school lacrosse coach. “His
maturity level was extremely high. Never experimenting with drugs and
alcohol. Almost fatherly to his brothers. Had a wonderful sense of humor.
He was a great teammate, very attentive and aware, very patient and kind.
A big-time leader on the team and in school—he could hang out with the
kids who were partyers and be in an honor-society meeting the next day.
Everyone loved him.”
Austin was taken to Inova Fairfax Hospital, where he died at 2
am on Monday. The entire community was stunned. The boy was beloved.
Football was beloved. In the Nokesville area, plans were underway to build
a new $850,000 youth-football complex; elementary-school students were let
out early on Friday afternoons, the better to high-five Brentsville High
players as they made their march down the town’s main road.
How could this have happened?
The Trenums went home. Later that day, their phone rang. Laura
O’Neal answered. She was Austin’s godmother, one of Michelle’s best
friends. She’d been there for Austin’s first birthday, eating
cowboy-themed cake; there when he got his first lacrosse stick, which he
carried everywhere, like a scepter. Now she would plan his
funeral.
There was a man on the line, Chris Nowinski, a former Harvard
football player, calling on behalf of scientists at Boston
University.
They wanted Austin’s brain.

The human brain is a wondrous thing. It enables us to throw a
football, allows us to breathe, think, and love. In its neurons and glial
cells, synapses and neurotransmitters, it is essentially who we
are.
And who we are is fragile.
Gerard Gioia opens his laptop. On the screen is a video
depicting a brain inside a skull. The brain, he explains, is a spongy mass
of tissue. Surrounded by fluid, it moves independent of the skull, just
slightly, the arrangement providing a protective measure of shock
absorption.
“And this,” he says, “is why the helmet will never be the
simple answer to this injury.”
Helmets prevent skull fractures but not concussions. Gioia
clicks a button. The head rocks back and forth. The brain smashes against
the inside of the skull. The screen flashes like a strobe light, a
comic-book pow! Such is the basic dynamic of a concussion, an
injury that occurs in football with alarming regularity: According to the
American Association of Neurological Surgeons, 4 percent to 20 percent of
high-school and college players will suffer one during a single season.
That’s likely a low estimate—some experts believe as many as eight of ten
concussions go undiagnosed.
“When the head or the body takes force, the brain moves,”
explains Gioia, head of Pediatric Neuropsychology at Children’s National
Medical Center and an expert on youth and adolescent sports concussions.
“It has a certain threshold, beyond which it stretches and
strains.”
Gioia loves football—played it himself in high school and
college. He wants to make the sport safer. Three weeks after Austin’s
death, he met with Gil and Michelle in his Rockville office, where a New
York Giants-themed street sign hangs on the wall. Michelle brought a
picture frame containing three photos of Austin, including one of him
joyfully painting his face before a volleyball game the week before his
death.
“Look at this boy,” she said, fighting tears. “Look at these
pictures. He wasn’t depressed.”
Shock giving way to despair, the Trenums wracked their brains.
Was there something we missed? They talked to Austin’s friends,
checked his text messages, read the journal he kept for English class:
I heard my favorite Sublime song. Today was good. I forgot to wear my
Hawaiian shirt. Bummer.
No angst. No suicide note. No sign that anything was wrong.
Nothing. The concussion, they figured—it had to be the concussion. But
how? Didn’t they go to the ER, keep Austin from strenuous activity, do
everything right? Scavongelli, the Brentsville High trainer, had
immediately pulled Austin from the game, protecting him from second-impact
syndrome, a rare but horrific condition in which athletes suffer a second
concussion while recovering from a previous one, causing rapid,
catastrophic brain swelling that ends in severe disability or
death.
After a concussion during his junior year, Austin was held out
of football practice for a week. A medical-hotline operator advised
Michelle to watch for signs of depression. She told Austin. He
laughed.
Oh, please, Mom.
“Why?” says Michelle. “Why did he do this? We must have said
that seven million times.”
• • •
A concussion is not a bruise. It’s a disruption of the
intricate system of electrochemical signals that constitute normal brain
function. Contrary to widespread belief, concussions don’t always coincide
with loss of consciousness. Symptoms include headaches, sensitivity to
light, confusion, lack of focus, irritability, and loss of interest in
favorite activities.
With rest and a gradual return to regular activity, most
athletes who suffer a single concussion experience no permanent ill
effects. Some, however, suffer post-concussion syndrome, in which symptoms
persist for months or years, in rare cases permanently. Having one
concussion may increase the risk of another. Multiple concussions are
associated with an increased risk of post-concussion syndrome as well as
depression and memory loss.
Think of your brain as a computer, Gioia says. The tissue is
the hardware, and the electrochemical signals are the software.
Concussions can scramble both, disrupting healthy equilibrium. Moreover,
they leave the brain drained of energy, like a cell phone with a bad
battery.
The best treatment? Rest—lots of it. Waking a sleeping
concussion patient every few hours to check for brain bleeding has long
been conventional medical wisdom, Gioia says, but actually is not a good
idea: You should check on them, but not disrupt their sleep. “The
essential aspect is allowing the cells to rebalance themselves.
Overworking the brain interferes with that recovery. And it’s not just
avoiding additional blows to the head. You can’t be out running. You need
good sleep. You have to manage school, any activity that involves a lot of
thinking.”
• • •
For 21/2 hours, Gioia and the Trenums talked, going over
Austin’s final weekend. As they connected the dots, two things became
clear: Football had injured his brain, which subsequently was overworked.
Texting. Video games. Driving. Studying. Staying up late. Normal teenage
activities. All of them too much.
Looking back over the weekend, they saw warning signs, subtle
indicators that something was amiss. Austin had trouble sleeping on Sunday
morning. He got lost on the way to Cody’s lacrosse game, even though the
directions consisted of a single right turn. He forgot what month it was
while fishing with his friend Carmen. He had “football
headaches.”
When Austin was concussed a few plays before halftime during a
football game his junior year, his teammates were the first to notice. In
the locker room, he couldn’t figure out how to work his chin strap and
began to bawl. Similarly, his final concussion left him cursing out his
best friend, Ryan Hall, for an on-field prank meant to make Austin
laugh.
Gioia showed the Trenums a diagram of the brain. He pointed out
the frontal lobes, about one-third of the total brain mass, the portion
just behind the forehead, where so much football contact takes place.
These gelatinous hunks of meat, he told them, are our executive control
centers. They allow us to reason, to choose right from wrong, to override
impulses, to connect current actions to future consequences.
In teenagers, the frontal lobes are still developing; in
everyone, they require a great amount of energy to function properly.
Damage or disrupt them, stretch them like Silly Putty, and concentration
suffers. Memory gets spotty. The systems governing emotion and reason are
thrown out of whack. You might forget how to work a chin strap; you might
consider that unbearably tragic. Nothing makes sense.
Austin’s parents believe that their son may have suffered as
many as four concussions during three years of playing football. Did those
injuries lead him to take his life? Gioia can’t say. There’s no direct
causation. The brain remains mysterious.
“My thought to the Trenums was that Austin’s brain wasn’t
functioning properly,” he says. “It was drained in terms of overall
energy, unusual emotional response was one of his manifestations, and the
argument about academics hit at that time. Bam! Those emotions go off, and
now the decision-making is not working properly, either.”
Meeting with the Trenums, Gioia was more succinct. He told them
Austin’s case was a perfect storm.
On the first snap of Brentsville’s first football game without
Austin, the school’s quarterback mimed a handoff to his absent fullback,
then took a knee. He pointed to the night sky, where cheerleaders with the
number 43 painted on their cheeks had released the same number of
balloons. The whole school wore white. Cody and Walker wore jerseys
bearing their brother’s number, 43, and watched from the sideline. At the
end of the game, a Brentsville player carried Walker off the field on his
shoulders.
Football went on. The Trenums understood. Gil, 46, had grown up
in Ohio and Texas, states where the sport is practically a religion;
Michelle, 48, was raised an hour and a half from Odessa, Texas, the
real-life setting of Friday Night Lights. She remembers pep
rallies and rabid boosters, caravans of cars with shoe-polish-painted
windows, what seemed like entire towns turning out for high-school games.
Gil and Michelle attended Texas Tech, where Austin went to summer football
camp. They loved the sport. So did Cody, a member of the Brentsville High
JV squad, and Walker, who played on a youth team.
As the Trenums grieved, friends and neighbors brought them
food, mowed and reseeded their lawn, even repainted their front door. The
family watched football. Tuesday nights. Thursday nights. All weekend
long. College and pro. Tackle after tackle, hit after hit. “I don’t know
why,” Gil says. “We just did. It was a distraction, something you had to
focus on.”
Gil and Michelle kept in touch with Gioia. They had donated
Austin’s brain to the Boston University scientists, who were studying the
effects of concussions and head trauma. The Trenums came to a frightening
realization: Like so many others around the country, the Prince William
County school system wasn’t doing enough to address athletic concussions.
What happened to Austin could have happened to anyone.
Six months before Austin’s death, Virginia had passed a law
requiring schools to educate students and parents about concussions and to
remove students suspected of sustaining the injury from the field of play
until cleared by a medical professional. In Fairfax County, education
meant watching a ten-minute online video; in Loudoun County, it meant
signing a two-page form. Prince William’s policy was still being written,
not scheduled to take effect until 2012.
A member of the Prince William County school board, Gil wanted
something quicker and better. A policy with teeth. He lobbied
administrators. He had Gioia make a presentation to the board, got input
from Nowinski, the former Harvard football player now with the Boston
University program. Spurred by his son’s death, Gil was
relentless.
Prince William’s new concussion policy went into effect in the
summer of 2011, mandating stricter return-to-play guidelines and more
thorough education for school athletic trainers. Students trying out for
sports are now required to attend an hourlong concussion seminar with at
least one parent.
“I have families contacting me all the time, telling me they
can’t thank Gil enough,” says Kendra Kielbasa, an advocate for
youth-concussion care and the wife of Austin’s former lacrosse coach.
Working with Gil to draw up a policy that stresses post-concussion
cognitive rest—the kind Austin didn’t know enough to get—Kendra had drawn
on her own experience. Her son, Connor, was concussed after being dropped
on his head during a seventh-grade wrestling match. Emergency-room doctors
checked Connor for a brain bleed and cleared him to return to school the
next day. Three weeks later, with his grades plummeting and his emotions
off kilter, he asked his mother if he could lie down.
“Sure,” Kendra said. “Why don’t you go to your
room?”
Connor looked around the living room. “I don’t know where it
is,” he said. “Can you take me?”
“The hardest part is that people don’t understand—your child
looks like he is fine, but he’s not,” Kendra says. “People have to
understand that it’s not just a bad headache for a day or two. And it’s
not enough to do [concussion education] in the high schools. We have to
bring it to the middle and elementary schools.”
Would more education have saved Austin’s life? The Trenums
think so.
Last fall, Cody played in a lacrosse tournament in
Williamsburg. Michelle was in the stands. A boy from another team was hit
hard and concussed. As his parents pulled him off the field, a woman
approached. She said she was a nurse. Michelle could overhear their
conversation. The boy was dazed, struggling to remember
things.
“Well, he’s not passed out,” said the nurse. “That’s a good
sign.”
Actually, Michelle thought, episodic amnesia is more of an
indicator of serious problems than passing out is.
The nurse continued to offer medical advice, much of it dated.
Michelle began to panic. As soon as the nurse left, she ran over to the
parents. “Take your son to a doctor,” she implored. “A neurologist. Get
him some rest. Keep a close eye on him.”
The parents asked, “Are you a doctor?”
“No,” Michelle said. “But my son died last year after a
concussion.”
“That scared them,” she says. “And all I could think was ‘At
least your son will live.’ ”
• • •
The brains come here, to a red-brick building in suburban
Boston. Each is weighed, photographed, and examined for signs of trauma
and disease, then carefully sliced in half. One half goes to the upstairs
laboratory, where scientists create tissue samples ten microns thin,
chemically stained and mounted on slides for microscopic inspection. The
other half is placed in a closet-size, stainless-steel freezer, preserved
for future study.
“There are more freezers,” says Victor Alvarez, a researcher at
the lab. “We’re always looking for more space.”
Football has a problem. The sport kills too many players. Some
slowly, some all at once. The evidence is in the freezers and in the
stacks of slides cluttering the office of Ann McKee, a neuropathologist
and codirector of the Boston University Center for the Study of Traumatic
Encephalopathy.
Each brain tells a story: former Pittsburgh Steelers lineman
Justin Strzelczyk, dead at age 36 after leading police on a high-speed
chase that began with hallucinations and ended in a fireball; former
college-football player Mike Borich, dead at 42 from a drug overdose;
former Philadelphia Eagles safety Andre Waters, dead at 44 from shooting
himself; former NFL safety Dave Duerson, dead at 50 from shooting himself
in the chest—specifically in the chest—after scrawling a note to
his family asking that his brain be donated to science.
Austin Trenum, dead at 17.
Concussion Care
After taking a forceful blow, athletes experiencing any of the following signs or symptoms should be removed from play and examined by a health-care professional trained in concussion evaluation.
The rule of thumb? When in doubt, sit players out.
Observable Signs
• Dazed or stunned appearance.
• Confusion about the game, player’s position, score, or opponent.
• Inability to remember instructions.
• Vacant stare or glassy eyes.
• Clumsy movements.
• Answering questions slowly.
• Loss of consciousness, even brief.
• Mood, behavior, or personality changes.
• Inability to recall events before or after the blow.
• Any seizure.
Self-Reported Symptoms
• Headache or pressure in head.
• Nausea or vomiting.
• Balance problems or dizziness.
• Ringing in ears.
• Double or blurry vision; seeing stars or flashing lights.
• Sensitivity to light or noise.
• Feeling sluggish, hazy, foggy, or groggy.
• Problems with concentration, thinking, or memory.
• Depression, sadness, irritability, or anxiety.
• Change in sleep pattern or trouble falling asleep.
After a concussion, athletes need physical and mental rest—no television, video games, music, reading, computer use, school attendance, or homework. Sleep is essential.
A return to regular activities should take place slowly after all signs and symptoms have resolved, under the supervision of a neurologist or other medical professional. Current medical guidelines call for a graduated series of monitored steps, in the following order, with each successive step allowed only if no concussion signs or symptoms manifest themselves:
1. Total rest.
2. Return to school half days.
3. Full return to school.
4. Light exercise (walking, stationary cycling).
5. Non-contact-sport activities and training (running, throwing).
6. Drills without body contact; light weight training.
7. Drills with body contact; heavy weight training.
8. Game play.
Sources: Centers for Disease Control and Prevention, 3rd International Conference on Concussion in Sport, Ontario Neurotrauma Foundation, TheConcussionBlog.com.
Last summer, Gil and Michelle came to McKee’s office. They
looked at slides of Austin’s brain. Through the microscope, they saw
axons, the long, slender fibers that connect nerve cells and conduct
electricity in the brain. In a healthy person, axons run together like
fiber-optic cable, straight and smooth. Austin’s were twisted, bulbous,
broken. In scientific language, it was a multifocal axonal injury; in
layman’s terms, the equivalent of frayed automobile wiring. Turn on the
radio and the windshield wipers might move; turn off the lights and the
whole car might shut down.
Michelle choked up. This, she thought, is my baby. This is what
ended his life.
Austin’s case isn’t unique, McKee says. There have been other
sudden, inexplicable suicides following concussions—some in the military,
some among high-school football players. Scientists are struggling to
understand the connection. But something is happening. Something
terrible.
“It’s the same pattern,” McKee says. “They have disordered
thinking and electrical impulses in the brain. They have a minor
irritation. And they just want to end it. It’s like having a fly in your
room and deciding to blow up your house.”
• • •
A decade ago, McKee wasn’t studying dead football players.
Nobody was. That changed when Bennet Omalu, a forensic pathologist and
neuropathologist, examined the brains of former Steelers linemen Mike
Webster in 2002 and Terry Long in 2005. Both had suffered slow, puzzling
descents into erratic behavior and madness, with Long ultimately killing
himself by drinking antifreeze and Webster dying of heart failure after an
extended period of living in his truck in which he sometimes shot himself
with a Taser gun in order to sleep and other times sniffed ammonia to stay
awake.
Omalu found that each had suffered from chronic traumatic
encephalopathy (CTE), a progressive neurodegenerative disease similar to
Alzheimer’s and linked to the absorption of repeated blows to the head, a
condition previously associated with prizefighters—in layman’s terms,
“punch drunkenness.”
Evidence suggests that CTE is caused not only by concussions
but also by subconcussive trauma. Little hits—the ones inherent in
football that occur on every snap, like the 1,000 to 1,500 hits to the
head that Boston University researchers estimate the average high-school
lineman takes each season, some at forces equivalent to or greater than a
25-mile-an-hour car crash.
CTE has been found in a number of deceased football players,
including Strzelczyk, Creekmur, Borich, Waters, Duerson, and Chris Henry,
a former NFL receiver never diagnosed with a concussion. Early stages of
the disease also were discovered in the brain of Owen Thomas, a
21-year-old University of Pennsylvania football captain who hanged
himself, and in Nathan Stiles, a 17-year-old high-school player from
Kansas who collapsed during a game and died of a rebleed of a brain injury
suffered in a previous game.
Because their brains are still developing, children and
adolescents are particularly vulnerable to brain trauma. A recent Virginia
Tech study measuring head impacts among seven- and eight-year-old football
players found that some hits generated more than 80 g’s of force, equal to
the blows delivered in college football.
“I think that in ten years we’re going to look back at this and
say, ‘Whoa,’ ” says McKee, who has examined thousands of brains over 26
years. “The public only knows some of the evidence. It’s overwhelming. And
as it accumulates, it’s impossible to deny.”
• • •
Austin Trenum showed no signs of CTE, none of the telltale
clusters of dark brown spots on slides of stained pinkish brain
tissue.
The sport damaged his brain nonetheless.
At a 2009 congressional hearing, Ann McKee presented a summary
of her work, acknowledging that hundreds of thousands of former football
players seem perfectly healthy. She then asked: Do we expect that 100
percent of cigarette smokers will develop lung cancer? Do we expect 100
percent of children who play with matches or even chainsaws will get
hurt?
Representative Ted Poe, a Texas Republican, said that parents
and players already know football is dangerous. He said government
involvement would mean “the end of football as we know it” because the
sport would end up becoming “touch football.”
Such are the terms of an ongoing national debate over
football’s safety and long-term viability, an argument that has
intensified since the May suicide of popular former NFL linebacker Junior
Seau. Mismanaged concussions can cause permanent harm and death. But even
players who never have a concussion are at risk of developing CTE. How
much is too much?
McKee is no abolitionist. She grew up in Wisconsin rooting for
the Green Bay Packers. Her favorite player was Willie Wood, a DC native
now suffering from dementia. Her two older brothers played the game. She
doesn’t want to end football; she wants to save the sport from itself.
Three years ago, she ran into a group of players from her daughter’s high
school at a doughnut shop outside Boston.
“So,” McKee asked, “you guys know anything about
concussions?”
“Oh, yeah,” said one of the boys. “I’ve had five.”
“I’ve had seven,” said another.
“It was a badge of honor,” McKee recalls.
For years, McKee loved attending prep football games. Not
anymore, she says. You just don’t know what will happen.
The room remains as it was. A lacrosse helmet. An SAT prep
book. A half-empty pack of gum. All on a desk. Austin and his friends
mugging in a photo booth, young and happy and full of life, the snapshots
tacked to a mirror. Clothes are piled on the closet floor, the bed unmade.
Sometimes Michelle will come upstairs and lie down, just to feel her son’s
blanket.
Downstairs is a bathroom. When Austin was in the hospital,
doctors working to save his life, Michelle tried to make a deal with God:
I’ll rip out the bathroom, make it bigger. Austin can be a vegetable
and we’ll take care of him. Just let him live.
“But I knew,” she says, her voice trailing off.
The first months were the hardest. Gil, a senior engineer at
SAIC, went back to work. The boys were in school. Michelle, a stay-at-home
mom, would lie on the living-room couch—the family’s golden retriever,
Biscuit, at her feet—and sob. Before Austin’s death, she had been
outgoing, involved in the community, digging up local land-use records and
political-campaign contributions to lead a successful fight against a
planned rock quarry. Not anymore.
She withdrew, felt vulnerable, couldn’t be around people who
didn’t know Austin. She threw herself into spy novels, then science
fiction, sometimes reading for seven hours a day. She had once favored
Anne Tyler and Pat Conroy, selections from Oprah’s book club. “But I
couldn’t read those,” Michelle says. “Nothing with mothers and kids and
emotions.”
When children take their lives, parents blame themselves.
Michelle wondered why she’d gotten on Austin about his homework; Gil
wondered why he’d let him do homework in the first place. A grief
counselor told Michelle it would take a year for the guilt to pass. “Even
I have trouble sleeping sometimes,” says Patti McKay, the Trenums’ close
friend. “I think about what Gil and Michelle saw. I don’t know how they
sleep. I can’t imagine living with that.”
Michelle still watched football, but not in the same way. She
winced at every big hit, noticed that concussed players almost always fell
with their forearms extended away from their bodies, a reflex scientists
call “the fencing response.” She began investigating sports concussions
and teen suicide, spending hours online, reaching out to military and
academic experts.
Researchers at the Centers for Disease Control and Prevention
tracked suicides, but they didn’t correlate those deaths with recent brain
trauma, never mind athletic participation. Nor did anyone
else.
Michelle befriended Dustin Fink, an Illinois-based athletic
trainer who runs a concussion blog. Fink’s anecdotal evidence suggested
that boys who played both linebacker and running back were at greater
brain-trauma risk. Michelle made a spreadsheet, one she still maintains,
logging every instance she could find of high-school and college football
players killing themselves: name, age, position played. She saw a pattern.
Linebacker. Running back. Linebacker. Running back. Just like
Austin.
• • •
Two football helmets rest on a table. One is black, matte and
battered, with an orange mouthpiece wedged in the facemask. The other is
reddish and gleaming, decorated with a skull and crossbones and a
breast-cancer-awareness sticker. Two gashes run down the
front.
The first helmet belonged to Austin. The second belongs to
Walker.
Michelle pushes them together. “This,” she says, “is how it
happens.”
It’s a Saturday, exactly one year after the weekend of Austin’s
death.
Cody finished the previous Brentsville High football season,
then quit. He didn’t say why. Walker continued to play for a youth squad,
fullback and linebacker, same as Austin. Gil and Michelle didn’t want to
overreact, give in to emotion, cocoon their son in bubble wrap. Besides,
Austin always took such pride in Walker. The boy loved to hit, so much so
that he bragged about it: Mommy, that kid is a baby. He cried, and I
didn’t even hit him that hard.
Walker wore a special chin strap, rigged with accelerometers
that measured the force of every blow he absorbed. If built-in software
deemed any hit powerful enough to cause a head injury, three green LED
lights on the chin strap would flash red. While Walker was making a
routine block, his head whipped sideways. Red lights. His coach pulled him
off the field. Two sideline nurses checked him out. Dizzy and frightened,
he cried.
“My head,” he said. “My head.”
The Trenums followed Gioia’s instructions. They made Walker
rest. They took him to a Sunday-night bonfire—a memorial for Austin—but
didn’t let him run around with his friends. On Monday morning, a
neurologist diagnosed Walker with a concussion. Sensitive to light and
sound, he was held out of football practice and gym class for a week. One
week after that, he was back on the field, Michelle looking
on.
“You’re so calm,” one of the other mothers said.
Michelle wasn’t. Watching football on TV was bad enough. This
was worse. Also, the chin strap. It was supposed to make things easier,
safer. But the lights kept turning red, once when Walker hadn’t even been
hit. Michelle made him sit out the entire game. Walker fumed, said he
wouldn’t wear the device again. Michelle sent the faulty chin strap back
to the manufacturer, got a replacement, then sent that one back, too. More
red lights. Was the problem a bad battery? Water leaking into the
electronics? Was the problem football?
Michelle wasn’t watching her son. She was watching the lights,
waiting for green to go red. She worried about punch-drunk football
players, the blows adding up over time—wondered if Walker’s concussion was
God’s version of a yellow flag. It was all too much.
Michelle Trenum kept coming back to the same
question.
“If you’re that worked up,” she says, “then what are you doing
letting your kid out there in the first place?
• • •
Losing a child, Michelle says, is like jumping from one train
onto another headed in the opposite direction. In an instant, you’re
barreling away from everything you once knew, farther and farther with
each second.
Brentsville High has a scholarship in Austin’s name. In their
living room, the Trenums keep a large photo of Austin, sweaty and beaming,
coming off a football field. On the ceiling above the kitchen table is a
spot with his fingerprints, smudged and faded, where he and his brothers
once liked to test how high they could jump. “I sometimes think we can
never repaint that,” Michelle says. There’s sadness in her eyes—green like
Austin’s—and pain.
“I love football,” Gil says. “I loved watching the kids play.
But it’s not the same anymore.”
Twelve years ago, Dallas Cowboys quarterback Troy Aikman
retired after suffering the tenth concussion of his Hall of Fame career,
the result of a vicious hit from Washington Redskins linebacker LaVar
Arrington. Aikman since has become a successful broadcaster, a man who
owes much to football. After the Super Bowl in February, however, he said
that the sport was “at a real crossroads. . . . If I had a ten-year-old
boy, I don’t know that I’d be real inclined to encourage him to go play
football in light of what we’re learning from head injuries.”
Michelle showed Walker the comment.
“I don’t think I want you to play football,” she
said.
He was upset—for a moment.
“Can I play another sport?”
Gil and Michelle are not against football. They don’t judge
others. But they’ve made their decision.
“As a mother,” Michelle says, “I’m a lot more relaxed watching
basketball.”
Patrick Hruby is a culture writer for the Washington Times and a contributor to ESPN.com and TheAtlantic.com, among others. You can contact him at patrickhruby.net.
This article appears in the August 2012 issue of The Washingtonian.